Incontinence, a condition affecting millions worldwide, is often misunderstood and stigmatized. According to the National Association for Continence, over 25 million adult Americans experience some form of urinary incontinence.
Incontinence can refer to several conditions and types, including urinary and fecal incontinence. This article will cover the most common causes of urinary incontinence.
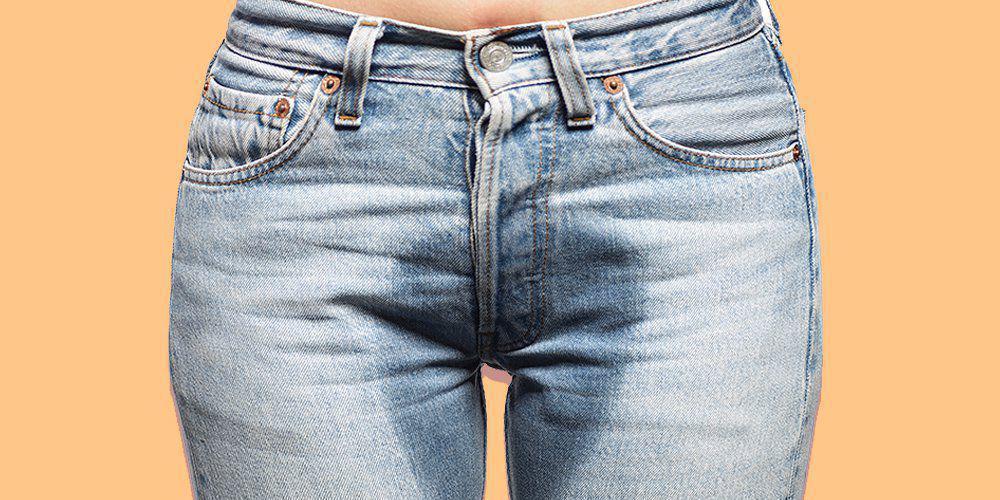
Urinary incontinence refers to the sudden involuntary leakage of urine, indicating a loss of bladder control. There are 6 different types of urinary incontinence, which manifest in different symptoms and arise from different causes.
Types of Incontinence:
Urge Incontinence (also referred to as overactive bladder or OAB):
Urge incontinence is characterized by a sudden and intense urge to urinate followed by involuntary leakage of urine
Stress Incontinence (sometimes called cough incontinence):
Stress incontinence is characterized by the unintentional loss of urine during physical activities that exert pressure on the bladder, such as coughing, sneezing, laughing, or exercising.
Mixed Incontinence:
Some people experience both stress incontinence and urge incontinence, and this is referred to as mixed incontinence.
Overflow Incontinence:
Overflow incontinence is most often experienced in men. It can be caused by a blockage of complete urine passage, which prohibits the bladder from emptying completely, thus causing leaks without the urge to urinate.
Functional Incontinence:
Functional incontinence happens when your urinary system can function, but other physical or cognitive impairments are causing bladder leaks.
Reflex Incontinence:
Reflex Incontinence is characterized by the release of urine with no warning or urge.
Pregnancy & Childbirth
Childbirth and pregnancy are significant contributors to urinary incontinence in women. The physical strain of childbirth can weaken the pelvic floor muscles and damage the nerves that control the bladder, leading to incontinence. Studies show that up to 40% of women experience some degree of urinary incontinence during pregnancy, and approximately one-third of women continue to experience incontinence after childbirth. These statistics highlight the importance of pelvic health and proper postnatal care to manage and mitigate incontinence risks.
Menopause
Menopause often contributes to urinary incontinence through hormonal changes that weaken the pelvic floor muscles. The reduction in estrogen levels during menopause can lead to significant alterations in the bladder and urethral tissues, diminishing their elasticity and resilience.
These changes increase the likelihood of urinary symptoms, making incontinence a common issue for many postmenopausal women. Proper management and targeted treatments can help mitigate these effects and improve quality of life.
Prostate surgery
Prostate surgery, particularly procedures like a prostatectomy, can lead to urinary incontinence in men due to potential damage to the muscles and nerves controlling bladder function. The removal of the prostate gland can weaken the pelvic floor and disrupt normal urinary control. Consequently, many men experience temporary or, in some cases, long-term incontinence following prostate surgery.
Pelvic floor damage
Pelvic floor damage beyond pregnancy and childbirth can lead to urinary incontinence due to factors such as chronic heavy lifting, obesity, and pelvic surgeries. These activities and conditions can strain or weaken the pelvic floor muscles, impairing their ability to support the bladder and maintain continence. As a result, individuals may experience involuntary urine leakage and a decreased quality of life.
Nerve damage
Nerve damage can significantly impact bladder control, leading to urinary incontinence. When nerves that signal the bladder and urethra are damaged, the communication between the brain and bladder is disrupted, causing involuntary urine leakage.
Common nerve conditions that frequently cause incontinence include multiple sclerosis, Parkinson’s disease, stroke, and spinal cord injuries. These conditions can impair the nerves’ ability to regulate bladder function, resulting in varying degrees of incontinence.
Medical conditions
Several other medical conditions can cause urinary incontinence by affecting bladder function and control. Conditions such as diabetes, urinary tract infections (UTIs), chronic constipation, and bladder stones can irritate the bladder and lead to involuntary urine leakage.
medications
Certain medications can contribute to urinary incontinence by affecting bladder control and function. Diuretics, commonly prescribed for high blood pressure, increase urine production and can overwhelm bladder capacity. Additionally, medications such as muscle relaxants and sedatives can reduce bladder muscle tone, leading to involuntary urine leakage.
Managing Urinary Incontinence
Managing urinary incontinence effectively involves a combination of lifestyle modifications, dietary adjustments, and reliable bladder protection products. Incorporating pelvic floor exercises, maintaining a healthy weight, and avoiding bladder irritants such as caffeine and alcohol can significantly reduce symptoms.
Additionally, using high-quality bladder protection products is essential for confidence and comfort. Because Market offers a range of products that are 37% more absorbent than leading brands, ensuring superior protection. These products, discreetly shipped directly to your door, cater to all levels of incontinence with absorbency options ranging from 1 cup to 6 cups, making finding the perfect solution for your needs easier.
Understanding the various causes of urinary incontinence is crucial for effective management and treatment. From hormonal changes and nerve damage to the impact of medications and other medical conditions, recognizing these factors can help individuals seek appropriate care and improve their quality of life. By addressing the underlying issues and exploring available treatments, those affected by incontinence can regain control and confidence in their daily lives.












Leave a Reply